The panel discussed various challenges and opportunities within U.S. healthcare, highlighting patient empowerment, improving healthcare education, the importance of monitoring diabetes, its connection to chronic conditions, and potential technological solutions to enhance healthcare. Their insights provide valuable perspectives on how patients, providers, and innovators can collaborate effectively to enhance healthcare outcomes in the U.S.
Okay, thank you for joining everyone. Welcome to the BOSTON LIVE WEBINAR hosted by BDMT Global. The BOSTON LIVE WEBINAR series was started during COVID in 2020, and this has been a major offering that has attracted many global innovators since then.
Today, we are introducing a special edition webinar on solving healthcare challenges, and we thank Orange Biomed, who is the sponsor and one of the featured speakers, as well as all who’ve joined to share their insights and those who are here to learn from this panel.
We’ll start with a brief introduction about BDMT Global as the host of the Special Edition BOSTON LIVE WEBINAR. And then our moderator, Stacey Simms, who is an award-winning author and podcast host, will guide the conversation around public and personal health so that everyone will have key takeaways after this webinar. You’ll learn about the current challenges and opportunities in U.S. health care, how communities can be involved, valuable advice for you individually and for your loved ones, why diabetes specifically is such an important issue, as well as what solutions and technologies are available and being developed. We’ll close with some exciting announcements, so please stay until the end.
So, moving on to our introduction, we have had many people joining the Special Edition BOSTON LIVE WEBINAR, including global innovators from different countries, healthcare leaders, and people who are interested in improving their health. We’d like to welcome you to share with us in chat, so send to the host and co-hosts where you are joining from, and if you have any questions, please post them in the chat as well. We’ll do our best to answer any questions by the end of this webinar, but since we’ve gathered many requests from attendees prior to the webinar, if we can’t get to all your questions, we will follow up with additional information.
While we’re facing challenges today, this is a good time in the U.S. to network and maximize collaborations across the ecosystem. It’s important to understand the entire global and healthcare ecosystem, and innovators often are not aware of the key players that affect the decision-making process. We provide educational opportunities and access to our connections, and this webinar is just one of the ways we share our insights and network. With the DAC movement and Global Connection Initiative, BDMT Global supports industrial and medical sectors in need of urgent transformation. And DAC has become a new growth channel for leading companies seeking global collaboration opportunities, including cutting-edge AI, healthcare, medical device, robotics, and automation innovators.
These are some of the KOLs who have been featured in our BOSTON LIVE WEBINAR series. As we have announced in our prior webinars, we are closing out applications for the Fortune Top 40 list of South Korean emerging healthcare innovations for the U.S. market. And we’ll be announcing more programs for others, so please stay tuned. And without further ado, I’m turning it over to Stacey Simms to introduce today’s featured speakers and to kick off this conversation.
So what I’d like to do is just ask the panelists to briefly introduce themselves and I’ll go around and start with the order that you are on my screen. I know it’s a little bit different for everybody, but Ny’Nika McFadden, would you please take yourself off mute and you go ahead and introduce yourself.
Dr. McFadden, thank you so much. Pat Meriwether-Argus, please introduce yourself.
Sure, thank you. John Robitscher. Hi, good evening.
Excellent job. Thank you. And Yeaseul Park, good morning.
Yeah, we have a lot to talk about. So let’s jump right in. And I’m looking at this first question. It’s just, you know, we’re trying to ease our way in here. But this one, let’s just jump on in and start talking about some of the biggest gaps in healthcare for Americans. I mean, we could spend the whole hour really with this one question. Dr. McFadden, let’s start with you. Just kind of take us through what you think some of the top healthcare challenges are in the U.S.
Absolutely. So unfortunately, Stacey, as you mentioned, we could spend a long time talking about this topic because there’s so many issues, unfortunately, within our health care system. But one starting with underinsured and uninsured. So as we know, insurance is very crucial whether you’re trying to prevent a chronic disease or if you’re simply trying to manage your chronic disease. That’s going to impact your ability to screen. It’s going to impact your ability to afford your medical supplies. And so we’re hoping that that will get better with insurance coverage. And also when we think about the access to quality health care.
For instance, if you live in a rural community versus urban communities. So, you know, some individuals may enjoy this environment where they’re not around a lot of people and being in a rural area, but it has its drawbacks because sometimes here in the U.S., if you’re in a rural community, you may be 50 miles or so from an accessible, well-equipped healthcare facility. And if you’re in an urban area, there’s a lot to do and you have top healthcare facilities, the drawback to that is sometimes the wait time to even get an appointment or to see the provider is for an extended period of time. And we know that’s risky with trying to manage your health.
Yeah. Pat, let me ask you pretty much the same question. What challenges rise to the top when you think about this question?
Oh, definitely access is one of the major issues, whether you’re in an urban setting shortage of healthcare providers, or you’re in a rural setting where there’s also a shortage and maybe distances as well. I also think that one of the challenges too is that it’s estimated 10% of all patients don’t get the proper diagnosis, or it can be delayed, it can be the wrong diagnosis. So having that sort of faith in the system to be able to have the correct diagnosis.
And then I also think about testing, for example, I’m in the Chicago area, and many people are on dialysis. And they’re on dialysis because they never got tested early on, they may have diabetes, they may have hypertension, and as a result, we see a disparity. A third of the population is African-American, yet 60% of the population on dialysis are African-American in Chicago. So those are some of the biggest challenges with the lack of standardization of testing, the access to testing, and the turnaround time to make an impact.
Wow, a lot going on there. John, let me ask you to weigh in, and all the panelists, as we go through this, please, you know, you can shoot me a message or just wave your hand. I want to bring everybody in, but I want to get through a lot of the questions as well. So I may jump around a little bit. If you have something to say, please let me know. Because I know you can answer all of these questions, all of you very well. But John, let me move on to having heard those, and we’re just scratching the surface, what are some of the opportunities then for health advocates and for proponents?
Well, I think there’s a lot of room for improvement in our healthcare system, even globally. It’s a fragmented system. We can do a lot more work collaborating together. I think some of the ideas around early testing, when Orange Biomed talked about having a home A1C. Those are the kinds of technologies we need to put in the hands of the patient or just the individual. They can help start to assess their healthcare needs. Many, many people in this country, seven out of 10 people, have multiple chronic conditions. And that coupled with an expensive system, they talked about a fragmented system. We really have to think carefully about how we access the system and how we put the power back in the hands of the individual so they can help advocate for their own healthcare.
Yeah. John, let me stay with you for this next question. Because we’re talking about when people are struggling, what specifically do you think they’re struggling with when it comes to chronic conditions? Especially as you said, so many have multiple chronic conditions. Are there some patient populations that are more or less aware?
Well, I think the access issue is a tremendous one. Dr. McFadden, I think, spoke on the access issue. And she is just spot on about the rural areas, there’s a lot less access. So you may not get to the provider you need. There’s less diversity in disciplines. You know, you might be a primary care doctor, but a lot of people with chronic conditions need specific health specialists. And then if you go to an urban population, you’re going to be waiting a very long time. I mean, it can take an urban population six months or more to see a specialist or even a primary.
So these are challenges that we have got to overcome in this system. But there’s a variety of things we can do, including some of the technologies you’re going to hear about tonight. And I think as terrible as COVID was, it brought us Zoom, which is what we’re on now. And I can tell you, at least half of my physician visits now are by Zoom. And I think that is a welcome strategy. I wish that this country would pay doctors appropriately for telemedicine, because I think it’s a great opportunity to bring more healthcare to more people.
Excellent. Dr. McFadden, let me ask you kind of the same question. You know, when you’re talking about a lack of access, and a lack of testing, you know, that’s got to affect being able to catch chronic conditions early. I mean, in the diabetes community, we see it all the time.
Absolutely. In public health, we talk about the three levels of prevention. So starting with primary, secondary, and tertiary. So within primary prevention, this is where we want to help healthy individuals to remain healthy. So for instance, we advocate for, please go to your provider every three months. Please make sure to get your vaccines. But within the secondary level of prevention, we understand at this point an individual is either at risk of developing a chronic condition or they simply are in the early stages of their illness. And so this is where we promote those cancer screenings. And then lastly, in tertiary prevention, this is where, unfortunately, an individual has lived with a chronic health condition that has impacted their quality of life.
So this is where we try to help public health professionals and say, hey, here are some ways to go through rehabilitation to try to improve your quality of life. And unfortunately, we’re trying to do better within the healthcare system to start advocating more for primary prevention. But with lack of access and quality healthcare, right, sometimes when we’re able to help an individual, they’re either at secondary or tertiary prevention level. And so it’s best to start at primary prevention as much as possible.
And Pat, just to kind of touch on that, you mentioned a little bit of that when you were talking about the situation in Chicago.
Right, wow. Yeaseul, let me ask you a question. You know, what are you observing in terms of results of testing for different populations? Does accuracy kind of vary among ethnicity or gender or age?
Yeah, sure. Let me talk about diabetes. Overall, diabetes prevalence in U.S. adults is about 11%, with communities of color hardest—almost 14% of Native Americans, over 12% among non-Hispanic blacks, and nearly 12% among Hispanic adults. In contrast, just about 7% of non-Hispanic white adults have diabetes. Regarding gender and age, men have slightly higher risk of developing diabetes, but women diagnosed with diabetes face greater complications, and prevalence rises steeply with age. 29% of those 65 or older are affected.
When interpreting A1C results specifically, some groups need extra caution. Traditional A1C tests can be skewed by hemoglobin variants, which are more common in Black, Hispanic, and Asian-American populations, increasing the risk of inaccurate readings in these groups from different backgrounds.
It is really a problem. Dr. McFadden, let me ask you this next question. We talked a lot about what patients are going through, but how do you engage patients? Can you talk a little bit about how you empower people?
That’s a great question. So we try to find the right balance of engagement. Sometimes patients are overly engaged, and they come to their appointments, and they have done a lot of surfing on the internet, and they are prepared to ask all kinds of questions. And some providers, I’m sure, appreciate that, and some may grow concerned. And so it’s finding that fine balance of trying to ensure that patients remain engaged, but to also get their information from credible sources.
And so ways to engage patients are to meet them where they are. So for instance, in a patient and provider interaction, you know, the patient may be concerned about their literacy when it comes to nutrition, whereas their provider may be fixated on their A1c. And that individual who, let’s say has prediabetes, they may say, okay, I understand numerically my A1c is not where it should be. What’s causing those issues in my opinion is I don’t really know what to eat. I don’t know where I should go to get healthy groceries. And so meeting that patient where they are and asking them what do they think personally their underlying root causes are of them being at risk of developing diabetes or heart disease, hypertension, any of the chronic health conditions that we know are prevalent here in the U.S.
But being able to address those questions, because then it opens the door for the patient to say, my provider is listening to me. My provider is going to give me more tailored advice versus this generalizable information and this packet that they’re going to hand over to me that I may or may not read. So meeting the patient where they are is so crucial in creating that safe space where they can ask any question.
I think this is a really important point. I really wish we’d flipped the system on its head and before a patient comes in, get their blood test work done early and then actually teach the phlebotomist. Those are the people who draw the blood. Teach them to say these are three questions you can ask your doctor and make them super general. But just to start the conversation, I think that’s one of the hardest things because it’s hard to talk to a doctor. It is. They’re wearing that white jacket. And even if you’re a professional like I am, you’re like a deer in headlights. You don’t know what to say, and you don’t want to appear stupid. So a lot of times you don’t say anything, and seven minutes later you’re out the door, and you really haven’t learned anything. And then you get home, and they give you your blood workup, and you can’t understand it. Their numbers are indecipherable.
So I really would love to see this work done more upfront so that patients could be engaged with their provider while in the office and saying, hey, my A1C, I don’t really know what that means, but it looks, this number seems high, it’s abnormal. What do I do? What does that mean? I really feel like we can do just so much more in just, you know, empowering people to be engaged in their own healthcare. And, you know, we have to start somewhere. And I think this is one area we can start.
Yeah, I mean, and then you get your blood work and you have to go back to the doctor anyway.
I’d like to add on to this, because I do think that there’s ways you can structure your office or your practice and work with patients in terms of co-development and co-production. And those aren’t just words, those are really activities. You can also have a patient family advisory council, which is now required in hospitals. And the other thing I always like to talk about is we talk about teach-back, and teach-back has always been the doctor or the clinician telling the patient about how to take their medication and then repeating it back.
Well, we like to talk about bi-directional feedback, teach-back, and that’s where the patient tells the physician their symptoms, what they’re feeling, how they feel that day, and the physician repeats that back to them and says, I understand, here’s how you’re feeling, and documents that. And that’s part of the diagnosis as well. That’s why we sometimes have so many problems with diagnosis, because the patient, and I did some studies with PCORI on this, and the patient says what they’re feeling, but it doesn’t get heard. It doesn’t get acted on. So again, I think there’s a way we can communicate better with each other.
And we’ve kind of touched on this, you know, some things that innovators can do and innovations that can happen. Yeaseul, let me ask you this question, you know, what do you see as ways innovators can interact with patients?
In the past, only professional healthcare professionals could perform some essential tests. And thanks to technological advances, we now have many different types of user-friendly at-home devices that deliver hospital-grade accuracy, allowing everyone, anyone, to monitor their health. So, as innovators, we need to focus on tools that help patients manage their own care, I believe.
Excellent. Yeah, so let’s talk a little bit about some of the biggest gaps in healthcare and how those can be addressed in the U.S. John, let me go back to you on this question because, I don’t know, these are such big questions, right? How can healthcare plans be more supportive?
Well, I think that we’ve got to come to the realization that a fragmented healthcare system is not a healthcare system that’s going to be really supportive. Health plans and insurance plans can go a long way in providing guidance to both physicians and the patients, as long as it’s done in a way that patients can access the information. We built a very simple app called HALT. It stands for Health and Lifestyle Training. And our idea is to put it in the hands of every single American. It can link with every kind of weight, scale, blood pressure, cuff, A1C monitor. But the idea is to make it really simple and accessible. And that’s where health care has not done a good job.
But when we can get there, and I would even say to just this point, even if the test is not 100% accurate, maybe there’s some inaccuracies in the test, at least there’s a starting point for a conversation. And I think we’ve all agreed that having a conversation is where it starts. And that’s where patients can learn more, get more information, interact with their physician and get, you know, get the correct information or get the correct test.
Dr. McFadden, let me ask you to kind of build on that. What is your advice if people are looking to monitor, improve their health? You know, there’s so much confusion, even once you’re diagnosed with something, this, the HALT app sounds great, something like that, you know, what, what would your response be?
Absolutely. So when it comes to, let’s say diabetes, for example, and you want to monitor your blood glucose level or blood sugar level at a single data point. It’s important to go beyond that single data point in instances, looking at the blood glucose or blood sugar trends. So, for instance, what I’ve often talked to patients about is within self-care monitoring, it’s important to use self-care monitoring to then help you use symptom interpretation. So meaning, what is typically causing your blood sugar to increase? What is typically causing it to decrease? So having patients to pay closer attention to monitoring any kind of changes within their symptoms is important.
And even if you, let’s say, do not have diabetes and you’re concerned about developing a chronic health condition because maybe you’re genetically predisposed and you’re at a higher risk of certain health conditions, What always helps me as a patient and what I tell everyone as a patient is within your notes app, you can always write down symptoms that you have been experiencing, the date of when it’s happening. Sometimes the time helps. As strange as this may sound, sometimes it helps to have pictures or images so that when you’re having these conversations with your provider and you can say, hey, you know, just to give you a heads up, I know we’re short on time, but I’ve taken a few notes about the symptoms that I have experienced over the past six months. I have some images. I know you’re the professional, you’re licensed to do this, but perhaps we can work together and here are some images to try to close in the gap of reaching a diagnosis together.
That is fantastic. Yeah, I mean, we all have our phones with us every second of the day. So I’ve started taking pictures of my medication and I made my husband do the same thing because I don’t know what milligram level I’m taking. So that’s great. Pat, kind of the same for you to kind of round out this part of the program here, you know, advice for individuals and understanding the risks for chronic diseases.
Well, you know, I think we had, I know John talked about the opportunity that COVID presented. There was another opportunity with COVID, and that was home testing. That became widely done. Medicare for the Medicare beneficiaries was sending out testing kits. It seemed like every few months you got more testing kits. But they had created the opportunity for people to believe in the home testing and to be able to know that they could do it themselves. And they had pretty pictures. Well, sometimes not so pretty, but pretty pictures that they follow along and they could do the testing. And so I think that opened up the door for home testing. And I have to say one of the challenges, I do work with oftentimes many seniors, that they live for that appointment that they’re going to for their checkup. So if they’re going in for A1C every six months, it’s like they build their hope that things turn out good around that. And there’s no testing in between. And so having the ability to test when you want to test, when you’re not feeling well, and like what you were saying, Dr. McFadden, is being able to track and trend what are the interventions or what are the things that really make a difference in your care.
So I think we can seize upon the opportunity because it truly is there and people are more than ready. And anyone that has diabetes, they don’t like to wait too long to get tested if they feel they’re not doing well. And if there’s not a clinician available, as John said, sometimes you can’t get in for, you know, six months to an appointment, this is really an opportunity to make an impact and to really make people feel well and also be able to track their care.
Yeah, let’s talk specifically about diabetes. I mean, you know, as I said, my son was diagnosed in 2006 with Type 1. But I realized then I knew very little about any kind of diabetes. And Dr. McFadden, let me start with you here. You know, do you think the general public like, do people know what diabetes is and it’s linked to other chronic conditions? I mean, I have my own answer from my personal experience, obviously.
In general, a lot of people know more about Type 2 diabetes and not enough about Type 1. I think we talk more about pre-diabetes, Type 2. We don’t talk as much about Type 1 and gestational diabetes. So if it’s OK with the panel, I would at least like to to have a brief overview of what are the differences.
So starting with Type 1, just because that’s the one that’s talked about the least, Type 1 diabetes is an autoimmune condition. So our pancreas pretty much has what we call beta cells. And the beta cells are supposed to release a hormone called insulin that a lot of us are aware of and so with insulin, it’s supposed to be administered or secreted through our beta in our pancreas to help regulate our blood sugar. Unfortunately, if you have Type 1 diabetes and it’s an autoimmune condition, the beta cells within your pancreas are damaged, and so they do not produce insulin as it should. So therefore, that’s why Type 1 diabetes is an insulin-dependent condition where insulin is required daily, whether it’s through self-injections, using a syringe, or a insulin pump, we also have wireless insulin pumps called a Omnipod that you may see sometimes on someone’s arm or leg as well as CGM to monitor their blood sugar levels.
Then with Type 2, this is the one that’s more common. We talk about this more often. Although it is tied to lifestyle factors based off of your engagement and exercise, the nutrition that you’re eating, it’s still important to talk about that some individuals can all of the right things, however some are still at a genetically higher risk of developing Type 2, which is why I also wanted to talk about pre-diabetes.
So pre-diabetes is you have not officially been clinically diagnosed with Type 2, however you’re at a high risk of developing Type 2. And so within pre-diabetes it all comes down to checking your A1c, monitoring what you’re eating, how often you’re exercising, and thankfully Type 2 is reversible. However, Type 1 is not reversible and currently there’s no cure for Type 1.
But then lastly with gestational diabetes, this occurs during your pregnancy. Now it’s important for individuals to know that although during your pregnancy, gestational diabetes can occur, after your pregnancy, you and your child are still at a higher risk of developing Type 2 diabetes. So we’ll have to do a better job of having those conversations with women that have gestational diabetes and say, hey, make sure you continually come back and get screened after your pregnancy.
That’s a fantastic definition. Thank you so much for taking us through that. I do still think that even with the Type 2 being the one that is more commonly discussed, I think there’s still so many, there’s so much misunderstanding about it. Pat, go over to you and just talk about like, you know, why is it important for people to understand that not only their risk for diabetes, but how it ties into other chronic conditions?
I gave the example of the chronic kidney disease. And that to me is one of the major challenges that we face is when people don’t understand the connections between different types of diseases. What is diabetes can lead to many different conditions. The one I’m most familiar with is the chronic kidney disease because that’s when they oftentimes end up on dialysis. And dialysis, there’s different time periods. It doesn’t last forever for patients. They don’t last forever on dialysis. They typically require a kidney transplant at some point. And unfortunately, there’s not enough kidneys around for everyone.
So I just, I always warn people that it’s important to get tested, deal with the results, you know, whatever the results are, it’s better than having to actually go on dialysis. And again, it’s not a failure. If you end up on dialysis, it’s something the way the disease progresses. So, but you know, there’s ways we can educate people on the connections between the diseases and people, you know, when you talk to them and they start talking about their neighbor or their family member or somebody that they heard about, that’s when it becomes very real for them when they can share and they can start internalizing this could happen to to me if I don’t do these things.
I think it was beautifully, beautifully said, you know, there are some new innovations out and Stacey is a mom of a Type 1. There’s a new drug out, FDA approved, T-Zeld, I’m getting the name wrong.
No, it’s right, it’s T-Zeld, you got it.
It delays the onset of, you know, temporarily delays the onset of Type 1, which gives moms and dads time to prepare for the diagnosis, Type 1 diagnosis, which, as I love to tell you, is jarring and fretful and stressful, both for the child and for the parents. And so I think this is a welcome opportunity of new technology to help Type 1s. Type 2 diabetes is the thing that we most typically deal with. And it really requires behavioral change. It’s figuring out ways to move more. I’m not going to say exercise because a lot of people with disabilities, and they can’t run or some can’t even walk, but we should find ways in which we can move more, maintain a healthy weight.
And, you know, just in America, I mean, I hate to say it, but all of us, we like our food and we like to feel like when we go to a restaurant, we’re getting our money’s worth. You know, it’s terrible. You know, it’s like, you know, we’ve been growing up on fast food, and we want the value meal. And it ends up being more calories than we you know, you could need to consume in a day or maybe even two days. And so we really got to get back to, you know, eating more nutritious, more whole foods, more nutritious meals, and, and then moving more, we’ve got to find ways in which we just can maintain a healthier body weight so that we can live those longer lives.
I mean, it’s so sad to hear Pat talk about a population in Chicago in the, you know, they should be dying at 85, not 62. And that’s terrible. That’s a terrible legacy that our healthcare system, you know, spends the most on healthcare of almost any other country in the world. And we would have results like that. It’s just tragic.
Yeah, so let me ask you about, as we’re continuing to talk about diabetes, the way it’s detected now, it seems like it’s a little late, right? Healthcare providers are quite often treating the disease when people have been symptomatic for a long time versus early detection. Can you talk about that?
Yeah, exactly. So today, most diabetes cases aren’t caught until a patient develops symptoms. Or routine labs flag an elevated A1C or fasting glucose. So to shift detection earlier, I believe we need proactive risk-based screening, offering at-home or community A1C test checks for those with family history, obesity, or other risk factors.
Well, what do you think about, just excuse me a second, what do you think about the, talk about this continuous blood glucose monitors. You know, many, many people, even health, completely healthy people are wanting to wear those more and more and you see them advertised. Do you think that’s a good trend or do you think that is a trend that may ultimately not be as helpful as other technology?
Yeah, I believe CGM is a really good tool for everyone, especially for those who have diabetes. And similarly, I think like A1C tests or glucose monitoring systems, you better have tests, right? It’s better than not doing anything. And especially it’s more valuable for people living with these chronic diseases and have higher risks, I believe.
Yeah. It’s a really interesting issue. I can tell you in the Type 1 community, when you want to talk about access and cost, and then we see athletes and people without diabetes wearing them, you know, for fun. Look what happens when I eat this apple. It’s really a bit controversial, but at the same time, it’s also becoming a way, as we talked about prediabetes, and I’m hardly the expert here. I’m a person in the community, but it’s, I think becoming an interesting way for people to understand their possible risk to Yeaseul’s point. You know, if you’re spending a lot of time above range, regardless of what you eat, you know, getting your A1C checked and talking to your doctor should really be on your list. It’s really interesting. I mean, and then we’re talking about detecting early. Oh, go ahead, John.
The GLP-1s have been so expensive. And the question is, you know, is that really a good technology for the general public? I’d sort of like to hear Dr. McFadden and maybe Pat ask the question to the two of them because you’re more immersed in the healthcare field. But, you know, it feels like it’s costs that would bankrupt this country if we tried to provide that kind of technology. But what are your thoughts?
It’s a great question. Pat, why don’t you go first? I will really have to keep it kind of short here. But it’s a great question. It’s worth going down. It’s so important.
I agree. I think the earlier the testing being done so that people can take precautions early on. I do have a question, because I actually do volunteer work at a children’s hospital. I am a bedside volunteer on Sunday mornings for 34 years. And I see many children that are diabetic. I mean, they’re young, very young. And so I’m wondering, you know, there’s the testing that’s done when a child is born, when a baby’s born, the newborn test There’s 36 tests that are performed with a few droplets of blood. Is there any way that can be detected, that diabetes could be detected early on like that?
I can answer that question. Well, the answer is unfortunately no, not from blood because it’s an autoimmune condition and it can develop at any time. You can do some genetic screening. Genetic markers and some, but in terms of just the prick of the blood that they do for newborns, you would catch some cases, because unfortunately, they’re even newborns and children who are very, very young. But for the most part, you’d have, I would love to see that, or at least a urine test at a, at the annual physical that every kid has to take before they go back to school.
Because I’m thinking, you know, thalassemia, sickle cell, all of those conditions, they identify them as newborns, you know, before they live hospital, they get the test results. So I just think there’s technology that could be developed.
So we’re talking about earlier detection, right? I mean, those are some simple ways that would be costly. We know that, but they wouldn’t be as costly as somebody going into diabetic ketoacidosis at age six. Yes, we’re kind of running around on these things. But let me ask you again, you know, obviously this A1C test might be a solution to earlier detection. Is that something that you think it would be working for?
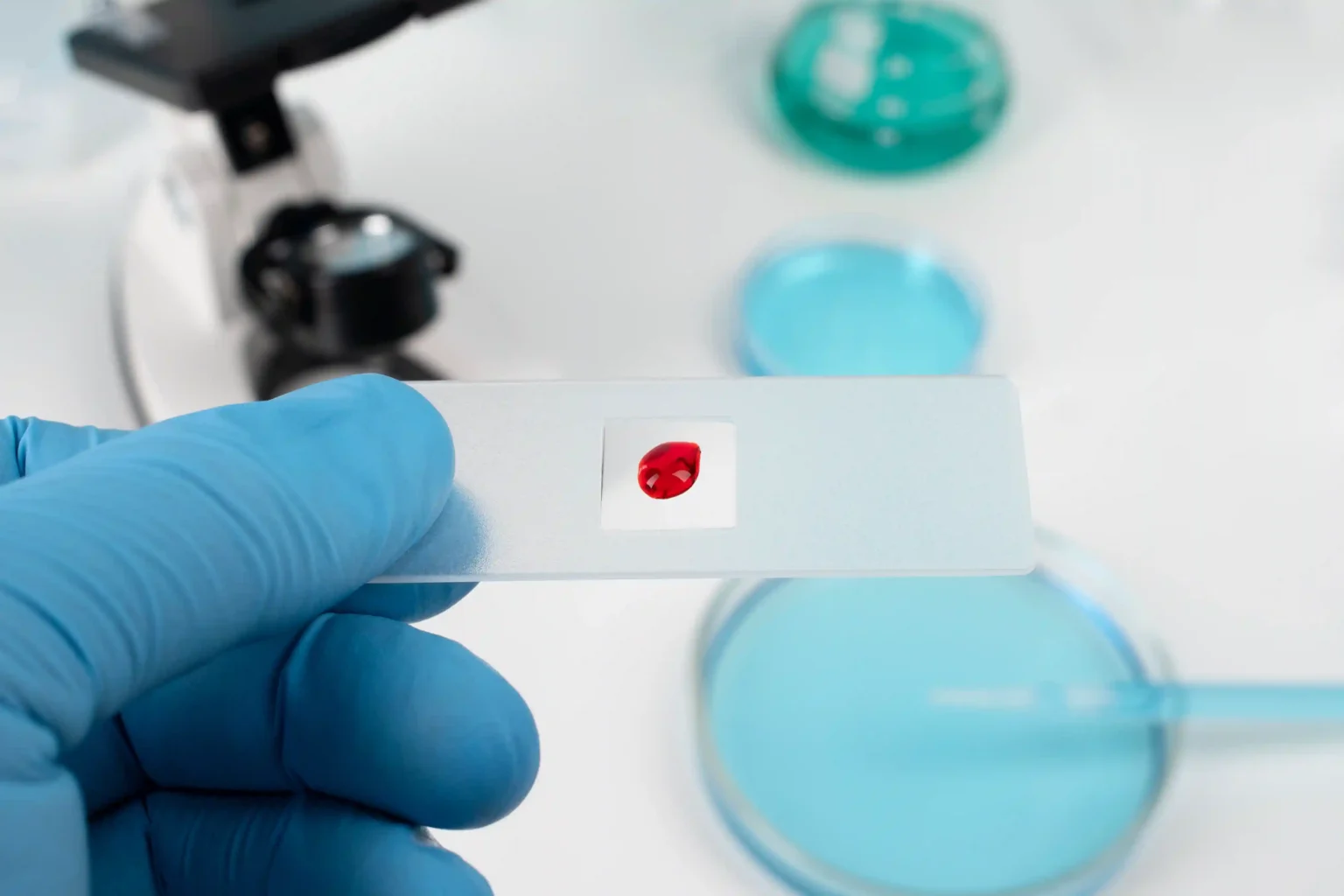
Yes, I believe so. A simple fingerprint test, just a single drop of blood is enough to assess your risk for diabetes. And with my family history, I always make sure to include an A1C test in my annual check. And if access to—if your clinic is limited or your situation makes it difficult, you can also pursue a home test kit to check your A1C always.
I’d love to hear what others think about it. I love that idea because I truly think that one of the challenges is also in different communities. Sometimes when you’re on Medicaid a payer that may be a little bit tough on testing. Sometimes they won’t test you for A1C early on. You know, you’ve got to be a certain age to get tested because that’s when it’s prevalent. And so I think having a home testing, affordable home testing is really going to be a pathway forward.
I agree. I think it’s a wonderful idea and it’d be great to put together a kit that could be sent to the home and, you know, just at least again, get that conversation started, initial baseline data on their, you know, their health. And it could go a long way to really supporting a lifetime of working towards a healthier lifestyle.
It’s hard to believe we’re coming towards the end. But I do have one or two audience questions I would love to get to. And I think this one’s really relevant. She says, I love John’s comment about learning how to speak to one’s doctor as a critical issue, you know, that many patients face, people get nervous. So I’m curious, and John, we will start with you on this one. What do you think about patients using ChatGPT, or other artificial intelligence to get their questions answered on the AI platform? Do you think it’s dangerous? Can you tell, I mean, I love this idea. I love this topic. John, what do you think of that?
ChatGPT is amazing. I probably use it every day in my administrative life of running a national organization. Put lots of questions through it. I would not use it yet for a strict diagnosis. It’s a good place to gather some information. You could ask ChatGPT if you’re set up to do it. What are some questions? I’ve got a high A1c, I think I might be diabetic. What are some questions I could ask my doctor? I think there’s some tools you can use for it, but I don’t, I wouldn’t necessarily, I don’t think we’re there yet as using that as your diagnostic tool for your health. Like if you put in your blood, your results from a blood test, I don’t know if you’d get as accurate as you would be, just get, you can type those things in there, get some information, and then go talk to your doctor. Say, even say, ChatGPT said, I’ve got this based on these results. What do you think? And then let the professional tell you.
Dr. McFadden, I saw you kind of chuckling. Your same thing, same kind of advice?
It’s great to start off as a tool, not complete reliance on it, but it puts you in the ballpark area of what kind of questions do I need to ask my provider? About to get properly diagnosed.
I mean, I think people are using it for all sorts of things and for diagnoses, which is kind of scary. But Pat, have you had an experience with, you know, not necessarily patients, but as you said, you’re in hospitals, you’re talking to people all the time. I gotta believe people are having conversations with AI about this stuff.
The way it’s being utilized sometimes is as a supplement to the discussion that goes on with the physician and a patient. So that ChatGPT is, and they call it different things in different systems, can also be a supplement to the discussion. The physician may have missed what a patient was saying, and yet they can enter into the diagnosis, not just for diabetes, but for other conditions as well. So I think that as an add-on, for the diagnostic discussion, I think it’s helpful. I’m the same way. If ChatGPT prescribes something for me, I would take it to my physician and ask.
Really quickly, we use AI coaching app because people are oftentimes accessing our app after, you know, it’s getting lifestyle change about physical activity. It’s interesting with AI. People tend to be a little bit more honest with AI than they are with their doctors, because it’s nonjudgmental. There’s no one who’s making any eye contact. They’re not raising their eyebrow or saying, oh, I wouldn’t do that. But it tends to be nonjudgmental. So I think there’s some things we could use. But ultimately, it is a tool for you to use with your, in conjunction with your doctor, not as instead of your doctor.
Yeah, it’s tempting, but I think that’s wonderful advice. Another question from our audience, and we’ve touched on this a little bit, but you know, how do we promote cause-based medicine as opposed to a symptoms-based approach in the U.S.? And I think this goes to a little bit of prevention as well. John, I’ll start with that as well? I mean, it’s such a big challenge. Do you think we’ll get there?
I think we could get there. I think we need to be we haven’t really talked about the social implications of healthcare in today’s society. As much as we spend on healthcare we’re probably the one of the countries that spend the least amount on transportation, housing, affordable housing, affordable food systems. And when those countries that spend a lot of money on the social infrastructure tend to have much healthier populations. And I know, Dr. McFadden, you deal with this every day in your in your practice. And you probably do, too. It’s where we need to be. I feel like we’re the richest country in the world and we need to get back to being the humble country that works overtime to help others. And I’d like to get back to that, because I think there’s a lot of infrastructure, social infrastructure, we need to build or rebuild to really have a truly healthy society.
Yeah, well said, well said. I do have a couple of quick wrap up questions. You know, we spent a lot of time talking about diabetes, of course, course, you know, how do you think the latest in healthcare in diabetes technology will help people with diabetes? I mean, I’ve seen, again, I don’t want to talk too much about Type 1, cause we do want to focus mostly on the larger population of Type 2, but it’s been 18 years since my son is diagnosed and the technology advances have been amazing. So let me start with you.
Like, how do you think this technology is really going to help people? A doctor here, but if I can say about it, in diabetes complication management, I believe two key biomarkers are blood glucose and A1c. So for blood glucose monitoring, the technology has evolved over decades now into CGMs integrated with insulin pumps to form autoimmune automated insulin delivery systems called AID. And until recently, accurate A1C testing was confined to hospital or labs. And now, an at-home A1C device is being compacted into a pocket-sized tool using advanced semiconductor and AI we’ve discussed about. So now, this innovation not only improves accessibility but also removes some inaccuracies from hemoglobin variants I discussed earlier that are more common in certain populations, so helping to narrow health care gaps as well.
Wow, that’s great. Pat, did you want to say something?
I just think that if we can provide home testing for people, that is a way to go. Many people work during the day. If I’m talking about some low-income communities, they’re not going to be able to take off during the day. They may be working in jobs that they can’t leave during the day. Their clinician may not be available at night. They may have family they’re taking care of And if we can start making it so it’s not only affordable but accessible to people along with, and I do believe there needs to be sometimes telehealth along with that, because I do believe that need to understand their scores and what it means and what they should be doing next.
If we could supercharge research, I believe there’s a cure within 10 years. I think there is a cure around the corner, but we need to supercharge research in diabetes, in cancer, in chronic disease and related risk factors. It’s just around the corner. We just need to find the answer.
And then Dr. McFadden, and let me ask you as we wrap up here, what do you see as the greatest opportunities to address healthcare needs in the U.S.?
I mean, there’s a lot of them. Absolutely. It’s 2025 now and technology is not going anywhere, which is great because technology at times can give us so much data, but it’s data that we need on improving our health. So when it’s all said and done, when we talk about diabetes technology? I think it’s so important that we use it to talk to our patients about maybe sick day plans, or if you’re engaging in physical activity, what setting should your pump be in? Especially if you’re concerned about hypo and hyperglycemia episodes, how do you properly use technology to try to keep yourself in range, especially when you have concerns about how do I resolve these problems? And if you don’t quite know, allow your technology to help you until you grow more confident in managing your care.
That’s great. We are out of time. Janice is coming back. Yes, I would love to wrap up. You were so wonderful. Thank you all so much.I mean, there’s a lot of them. Absolutely. It’s 2025 now and technology is not going anywhere, which is great because technology at times can give us so much data, but it’s data that we need on improving our health. So when it’s all said and done, when we talk about diabetes technology? I think it’s so important that we use it to talk to our patients about maybe sick day plans, or if you’re engaging in physical activity, what setting should your pump be in? Especially if you’re concerned about hypo and hyperglycemia episodes, how do you properly use technology to try to keep yourself in range, especially when you have concerns about how do I resolve these problems? And if you don’t quite know, allow your technology to help you until you grow more confident in managing your care.
That was really great. And we have a few slides and announcements, like we mentioned, we would wrap up with. And thank you all for sharing your questions. If we didn’t get to them, as mentioned earlier, we will wrap up and send follow-up with people who have additional questions. Feel free to chat or email, and we’ll address them after the webinar as well. And as we wrap up, thank you, Stacey and your panelists for sharing all of your insights. I’m sure the audience will have some key actions and takeaways from this conversation. So let’s move on to the next slide and we’ll wrap up this section of the webinar with next steps and our special announcements. So as mentioned earlier, Orange Biomed announced today the launch of their nationwide campaign, M.A.P. Your Health. The campaign is aimed to empower community members to monitor the risk factors for chronic disease in collaboration with local and national health care leaders. Yeaseul, can you say a few words?
Sure. So thank you, everyone, for joining today. We look forward to seeing people who will be at the American Diabetes Association Conference in coming June and meeting people in Chicago at our August Map Your Health local event. Thank you.
Thank you, Yeaseul. Now, if you move on to the next slide, we’ll share it with you. This link again, map.orangebiomed.com is where you can join the M.A.P. Your Health movement and more announcements will be shared here with tailored resources and connecting with community partners here.
And if you could stay on for a few more minutes for those of you who are able to, I’m just going to go through a few slides of some of the community partners and campaigns that are relevant that are shared on this M.A.P. Your Health Community Education Portal. So the next slide shows this reversing prediabetes. So if people are not aware of your prediabetes risks, we encourage you to share this with your loved ones. It’s a Do I Have Prediabetes Ad Council campaign, where you’re encouraged to take a one-minute risk test. And organizations are encouraged to share this, and everyone can pass it along to understand whether you might have a risk of prediabetes.
This next resource is from the Academy of Nutrition and Dietetics, and they have a diabetes dietetic practice group that specializes in diabetes care. And this is also featured on the M.A.P. Your Health campaign website. Dietitians are critical to help you improve your health and prevent chronic diseases. So this is another community that we’re engaging with. And then on the next slide, as our speaker, John Robitscher, mentioned earlier, the HALT Chronic Disease Platform is a great resource for healthcare providers and individuals to become empowered to prevent disease. And so they have this app-based solution that John talked about with eight programs on one platform, app-based and accessible to take better control of your health and become an advocate of part of the M.A.P. Your Health movement as well.