

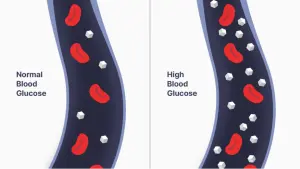
In 1958, Huisman and Meyering employed chromatographic techniques to isolate hemoglobin A1C from other hemoglobin variants (1). Key achievements in A1C testing to date are summarized below.
Samuel Rahbar initially reported the association between its elevation in diabetes in 1969 (2).
Anthony Cerami, Ronald Koenig, and their team suggested in 1976 using hemoglobin A1C as a marker for monitoring glucose metabolism control in diabetic patients (3).
Commercially available laboratory-based hemoglobin A1C testing became available in 1978.
Point-of-care (POC) hemoglobin A1C testing became available in the 1990s and usage has increased over the last decade.
A committee of international experts recommended A1C testing be used as widely as possible to diagnose diabetes instead of the blood sugar test at the American Diabetes Association’s 69th Scientific Sessions in 2009. (4)
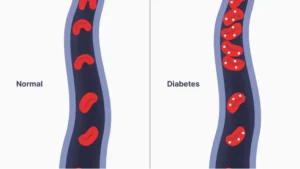
Today, the test is a critical component for diabetes diagnosis, treatment and management (5).
Yes, the HbA1C test and A1C test are the same. The A1C test is also referred to as the hemoglobin A1C test (6) and Hb stands for hemoglobin.
A recent study by the University of Florida revealed that at-home meters currently sold over the counter (sold under generic pharmacy brands or A1CNow+ brand, a subsidiary of SinoCare International, based out of Hunan, China) are not as accurate as traditional laboratory equipment (9).
OBM rapid A1c achieves the same level of accuracy as traditional laboratory test equipment. The device was designed to use a completely novel testing method (measuring physical properties of red blood cells using microfluidic technology) to overcome accuracy challenges with current at-home A1C tests or POC devices on the market.
See a full comparison of OBM rapid A1c vs. traditional at-home and laboratory testing equipment here.
Hemoglobin variants are one of many factors that can influence an A1C test’s accuracy. This type of variant is most commonly found in patients of Black, South and Southeast Asia, and Mediterranean descent. Measurements for these patient populations may not be entirely accurate (10).
In addition, other factors can affect A1C result accuracy in some ethnic group. For example, the Black population has a higher rate of sickle cell disease, and A1C test result for people with sickle cell disease are significantly inaccurate.
Read more about minority patient groups’ higher risk of developing diabetes and receiving inaccurate A1C readings.
A1C meters can be purchased in-person at most pharmacies and online directly through manufacturers’ websites.
Orange Biomed is currently conducting U.S. clinical trials of OBM rapid A1c and aims to obtain FDA clearances in 2025.
Sign up here to receive updates on U.S. clearance and commercial availability.
Reimbursement information will be released for the OBM rapid A1c system after FDA clearance is received (anticipated for 2025). In the meantime, please contact us with any questions.
(The reimbursement for the OBM rapid A1c At-Home System may vary depending on your insurance plan. Please reach out to your insurer for more detailed guidelines.
Additionally, the OBM rapid A1c At-Home System purchased over the counter is eligible for HSA/FSA reimbursement.)
1.“Chromatography of hemoglobin types on carboxymethylcellulose.” National Library of Medicine. Read More
2.”Structure of hemoglobin A1c: nature of the N-terminal beta chain blocking group.” National Library of Medicine. Read More
3.”Correlation of glucose regulation and hemoglobin AIc in diabetes mellitus.” New England Journal of Medicine. Read More
4.“Standards of Medical Care in Diabetes—2009.” American Diabetes Association. Read More
5.“Understanding A1C Test.” American Diabetes Association. Read More
6.”The A1C Test & Diabetes.” National Institute of Diabetes and Digestive and Kidney Diseases. Read More
7.“Differences in A1C by Race and Ethnicity Among Patients With Impaired Glucose Tolerance in the Diabetes Prevention Program.” National Library of Medicine. Read More
8.“A1C chart and understanding A1C levels.” Medical News Today. Read More
9.“Some in-home tests for average blood sugar levels less accurate than traditional method.” University of Florida College of Medicine. Read More
10.“The A1C Test & Race/Ethnicity.” National Institute of Diabetes and Digestive and Kidney Diseases. Read More
CV<2%
CV>3.5%
CV<2%
(Not applicable)
No tolerance
Not Affected
Disposables
Disposables
Lifetime-long Reusable
(Not applicable)
2-5 days (mail-in)
5 minutes
5 minutes
(Not applicable)
4 months
24 months
0.3ml (300µl)
0.005ml (5µl)
0.005ml (5µl)
$79-89
$16-33
TBA
Stay informed about our launch and get exclusive updates straight to your inbox. Fill out the form below, and we’ll make sure you’re among the first to know when OBM rapid A1c test hits the market.
"*" indicates required fields