New Blockbuster GLP-1 Opportunities
The New Reality of Use Case Zero - Diabetes Management
GLP-1 Discontinuation Rates: Summary of Published Studies
| Patient Population | 1-Year / 3-Year Discontinuation Rate | Source |
|---|---|---|
| Patients with Type 2 Diabetes (using GLP-1 RAs) | 23.6% at 1 year; 38.5% at 3 years | Diabetologia , (2025) |
| Patients with Overweight/Obesity (using semaglutide for weight loss) | 64.8% at 1 year; 3-year data not available in study | JAMA Network Open (2025) |
| Older US Adults with Diabetes (on Medicare, using injectable semaglutide) | 59.5% at 1 year; 3-year data not available in study | JAMA Cardiology (2025) |
The Two Pillars of Lapsed GLP-1 Adherence

1) The Strategic Shift to GLP-1 Pills and Patches to Fight “Needle Phobia”
2) Visible Results and a Positive Feedback Loop to Cut GLP-1 Discontinuation
Why GLP-1 Adherence Remains a Critical Challenge
Despite the rapid growth of GLP-1 therapies, long-term patient adherence remains a persistent and under-addressed challenge. While these drugs deliver strong clinical outcomes, real-world data consistently show high discontinuation rates within the first year of treatment.
Several factors contribute to this drop-off. Injection fatigue and needle aversion continue to deter many patients, while others lose motivation when visible results plateau or when ongoing progress is difficult to track between physician visits. Cost and access barriers may further compound the issue in certain populations.
As GLP-1 therapies expand into broader cardiometabolic indications, improving sustained adherence is becoming a critical priority for providers, payers, and pharmaceutical companies alike. This creates a growing need for patient-centric tools that can reinforce engagement and provide clear, ongoing feedback on treatment progress.
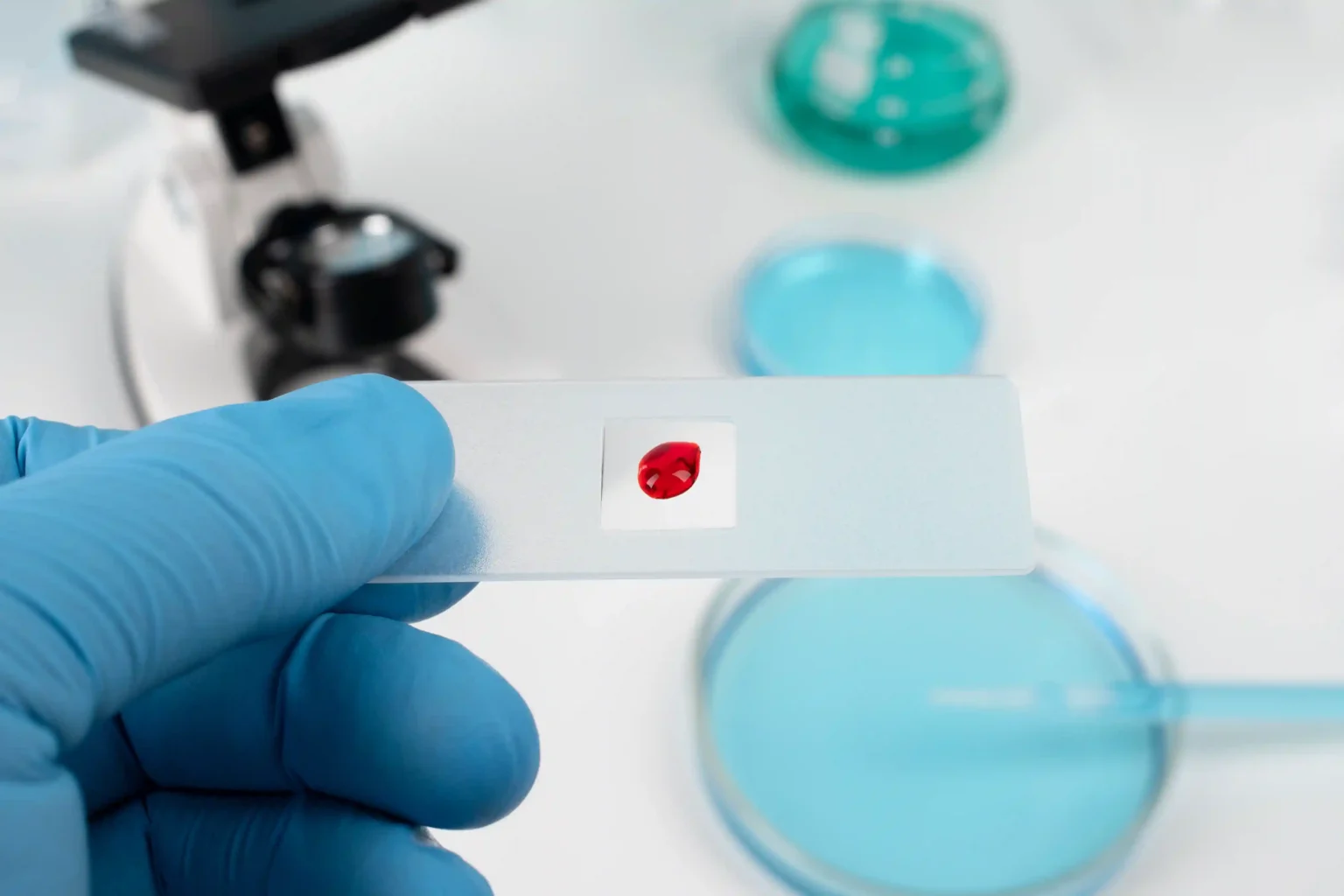
How to Improve GLP-1 Adherence with an At-Home A1C Test
Patients can improve GLP-1 adherence by using a portable A1C test to obtain immediate, tangible proof of progress. Instead of solely relying on semi-annual doctor’s visits for feedback, patients can now directly observe the results of their commitment. This regular, quarterly confirmation of progress—seeing their A1C numbers fall or stay low—can help serve as a powerful motivator, validating their efforts and reinforcing the value of staying the course with their treatment plan.

The Augmented Portable A1C Device: The Critical Data Link
- From Diagnosis to Continuous Management: The OBM rapid A1c meter is a tool to support the new era of care. It is being designed to enable convenient, regular checks of the gold-standard metric for long-term glucose control (the A1C test), which is crucial for managing chronic conditions.
- The Power of At-Home Testing: Moves diabetes management along with the market trend toward at-home testing. Our portable device aims to provide immediate results anytime, anywhere—within patients’ homes, on the road, and other settings—supporting more proactive patient monitoring and informed discussions with providers based on results. This aligns with the larger digital health trend of moving care out of the lab and closer to the patient.
- Generating the Data Ecosystem: This is the key value proposition. Our device has the potential to generate a continuous stream of lab-quality A1C data. This data can help:
- For Providers: Monitor the effectiveness of GLP-1 therapy and guide treatment decisions.
- For Payers: Provide tangible evidence of a drug’s success in improving patient health outcomes and demonstrating long-term ROI, which is crucial for justifying the high cost of therapy and supporting value-based contracts.
- For Pharma Companies: Offer real-world evidence on drug performance.
The Payer's Imperative: Demonstrating Long-Term Value and ROI
What Can You Do for GLP-1 Adherence and Patient Adoption Acceleration
- Increase Patient Lifetime Value (LTV): By improving adherence by even a few months, the revenue from a single patient increases substantially, far outweighing the marginal cost of the test.
- Differentiate in a Crowded Market: As more GLP-1s enter the market, providing a proven adherence solution becomes a powerful competitive advantage and value proposition for payers and providers.
- Generate Real-World Evidence (RWE): Aggregated, anonymized A1C data provides powerful RWE on drug performance in a real-world setting, supporting value-based contracts and marketing claims.
- Direct Patient Relationship: It creates a channel for education, support, and loyalty, moving beyond a purely transactional relationship with the healthcare system.
- De-risk Payer Negotiations: Providing tangible, objective proof of glycemic efficacy directly addresses the payer’s demand for demonstrated ROI, facilitating better formulary positioning and reimbursement.
Partner with Orange Biomed
FAQs
- Psychological Profile: A history of all-or-nothing thinking, low frustration tolerance, or previous discontinuation of other chronic medications.
- Social Determinants of Health: Unstable housing, food insecurity, or low health literacy.
- Clinical Presentation: Expressed anxiety about injections or a primary motivation driven solely by a single event (e.g., a wedding) rather than long-term health.
- Early Treatment Response: Patients who report minimal side effects and minimal perceived benefit in the first 3 months are at a significantly higher risk of lapsing.
10. Are there tools or technologies that can improve adherence to GLP-1 medications?