In 2023, the U.S. healthcare system still faces many challenges and gaps in care for those with diabetes and prediabetes. How can providers increase awareness of prediabetes through better practice efforts? Keep reading for more information.
Gaps in Diabetes Care Stem from Lack of Awareness of Prediabetes… And Less Action to Catch it Early
The U.S. has exceptionally high diabetes rates and even higher rates of health complications that result from it. More specifically, according to Spectrum News 1, the South has one of the most significant percentages of diagnosed diabetes.
A diabetes diagnosis and proper treatment reduce the risk of long-term health complications. A prediabetes diagnosis can have even better results in preventing complications. But how can healthcare professionals help their patients recognize the signs and catch them early?
Dr. Stef Alexopoulos, an endocrinologist at Duke Medicine, helps us understand how U.S. healthcare professionals and patients can do better.
Dr. Alexopoulos, who has been working in the Southeast for nearly a decade, explains that there are instances when the issue is the gap between knowing how and when to take proactive steps and making sure the people at risk have the information that they need to be fully aware.
“I can’t tell you how many times I have seen people who either have prediabetes and don’t know about it because no one told them it’s on their blood test. Or someone who comes to me for (a) new diabetes (diagnosis) and have had prediabetes for years, and when I ask them, they say that no one had told them that they had prediabetes for years,” Alexopoulos said. “If you don’t give people that opportunity then they will just progress down that path.”
U.S. healthcare professionals can prevent the development of complications and higher diabetes diagnosis rates by ensuring the people who are at risk are properly educated.

Preventing Complications is Doable. However, Some Patients Can’t Afford Healthcare Until it is Too Late.
Dr. Alexopoulos made a critical discovery regarding prediabetes and early diagnosis when attending clinical training through an Emory University Residency at Grady Memorial Hospital in Atlanta. This hospital was a medical safety net, meaning it admitted patients regardless of their ability to pay.
Dr. Alexopoulos says, “Seeing firsthand the amount of patients who had completely preventable complications and especially those of socio-economic disadvantage. It felt crazy to me like it really ignited a passion in me to really try to do something to improve the health of people with diabetes.”
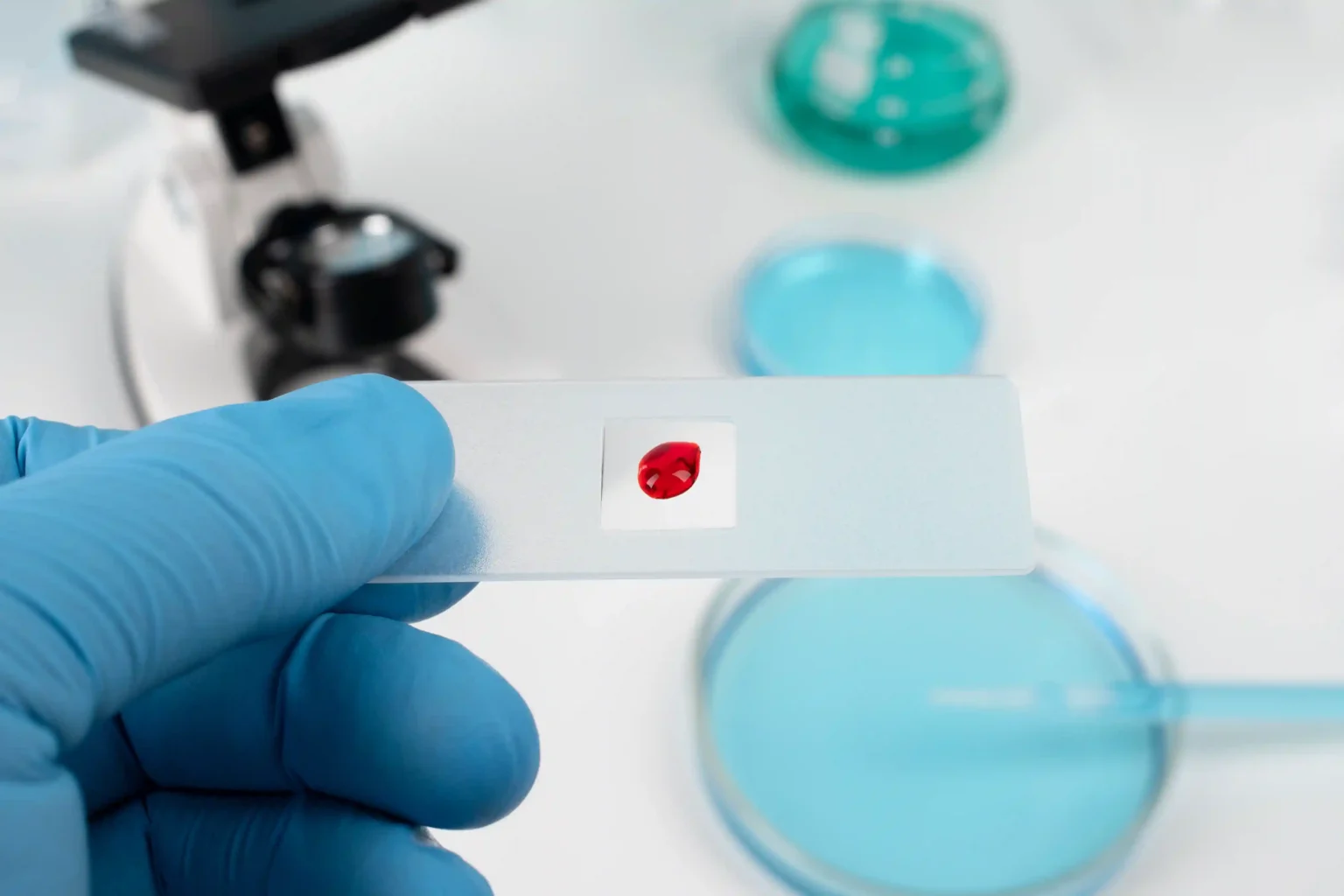
Prediabetes is defined as a health condition where a patient’s blood sugar levels are higher than they should be but not yet high enough to grant a type 2 diabetes diagnosis.
This condition is common yet frequently goes unnoticed or undiagnosed until the patient receives a type 2 diabetes diagnosis because of a lack of awareness. “We just see too much of these things when we know they can be prevented,” Dr. Alexopoulos said.
What startles Dr. Alexopoulos the most is the number of complications tied to diabetes after diagnosis. She explains, “Limb loss, people being on dialysis, having neuropathy from diabetes, having really bad liver disease.” Thus, U.S. healthcare professionals need to take more action to educate their patients, especially in the Southern states with higher risk and need.
How Can U.S. Healthcare Professionals Take Action to Educate Patients At Risk and Catch Prediabetes Early?
Dr. Alexopoulos provides some critical steps that U.S. healthcare professionals can take to address these gaps in care for patients with prediabetes and diabetes–diagnosed or not.
The first step is meeting patients where they are in their current life and health status. “We’re trying to work with what we have and make sure that we improve the lives of people with diabetes,” she emphasized.
Step two involves improving the patient’s quality of life. Encouraging at-risk patients to develop robust health habits such as monitoring A1c levels, taking oral pills, and checking their blood pressure are a few actions you can do to ensure they are receiving proper care. “A big focus of what diabetes management is all about is trying to prevent the complications,” she said.
The key to diabetes management and prevention is consistency. If you can encourage your patients to keep a consistent health routine that will ensure benefits to their overall quality of life, then consider that a win.
Follow the Orange Biomed social media pages for more information and updates on how you can help your patients.
Source :